Læs og kommenter bloggen på Simon Tullochs Linkedin
The connecting theme of the two papers, and much of the work I have been involved in over the last few years, is how to involve patients in healthcare improvement, management, evaluation and research in a meaningful way. Aiming for partnership, whilst avoiding manipulation and tokenism. To ensure meaningful patient involvement, infrastructure is critical, otherwise patient contributions to healthcare provision are likely to be superficial.
Læs artiklerne her:
Increasing the understanding of mental illness and helping to establish a dialogue
NB: I will use the term ‘patient’ in this blog. However, I often use ‘service user’, ‘citizen’ or even ‘expert by experience’. Which is the correct term is beyond me, and appears to change over time and depending on who I speak with. For the sake of consistency, I will stick with ‘patient’ hereafter.
Indlæggene skrives af forbedringsagenter, der er ansat hos eller samarbejder med Dansk Selskab for Patientsikkerhed.
Formålet med bloggen er at dele erfaringer med og fremme dialog om forbedringsarbejdet.
That’s nice
We have been talking about ‘patient involvement’ in healthcare for many years. Most healthcare professionals agree it is the right way of working. Over the years, I’m sure many of us will have been to healthcare conferences where the subject is discussed, and patients may even have been wheeled out to share their experience of ‘being involved’. That’s nice.
As a result of seeing these talks, some people may even have been inspired to read more about the subject, for example here: (http://www.ihi.org/communities/blogs/Pages/default.aspx#PFCC). That’s also nice.
But what difference does that make?
Mind the gap
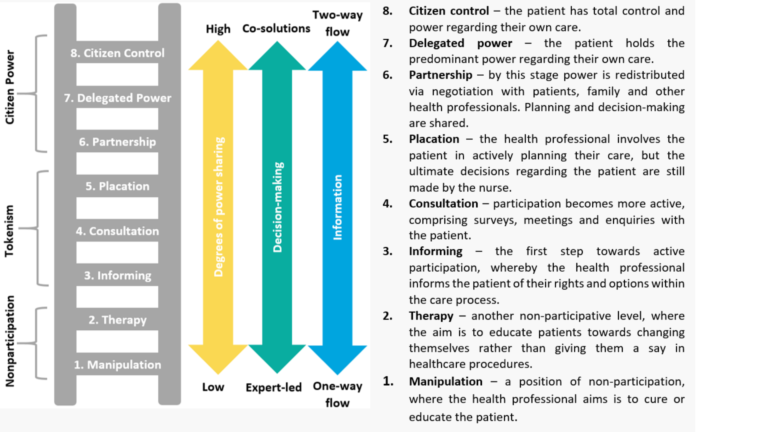
For me the issue focuses on how health professionals can cross the gap between ‘that’s nice’ to ‘that’s the way it is’. There are several models to help us better understand ‘patient involvement’. One of the most well-known is the ‘Ladder of Engagement and Participation’ based on the work of Sherry Arnstein (1969). This model sets out the different forms and degrees of patient involvement, indicating that patient activity only really becomes meaningful at the top of the ladder.
The Ladder also helps health professionals identify and understanding the power imbalance between themselves and their patients. Whilst this model was developed specific to clinical care and interaction, the principles apply across all elements of healthcare provision.
The eight levels of the Ladder, from the bottom rung and progressing upwards, are as follows:
What are the chances?
The involvement of patients in the two research projects linked to the two papers didn’t happen by chance. Where I used to work – East London NHS Foundation Trust (ELFT) – has systems in place to ensure patients (and their carers/family members) are involved in all aspects of healthcare delivery, including research and quality improvement.
A crucial element of this infrastructure is the work undertaken by the ‘People Participation Team’ (https://www.elft.nhs.uk/Get-Involved/People-Participation) who describe their role as “helping our service users and their carers to have a say in how we run the Trust. But more than that, it is also about working together so that we can offer a better service for all … We want our service users and carers to get the very best services. We can only do this by listening to you and working with you to make sure we deliver what you want. That’s why your voice is so important.”
As a result of this infrastructure, patients are involved in all aspects of service provision including: selecting prospective staff (from the domestic staff through to the Chief Executive Officer), training staff, undertaking audits, collecting patient feedback data, members of quality improvement projects, developing and agreeing strategy documents… the list goes on! At this point I should also mention that ELFT is primarily a provider of mental health services, many of the people involved in this work have a history of mental ill health. This has never been a barrier to involvement.
Nothing about us, without us
ELFT also has strong relationships with several academic partners. One of these partners (City University London) has a ‘Service Users and Carers Group Advising on Research’ (SUGAR: https://blogs.city.ac.uk/sugar/). The group was founded in 2009 by Professor Alan Simpson and his colleagues in mental health nursing as they were “keen to further develop service user and carer involvement across their programme of research and build long-term collaborative research relationships with members of local communities in east London.”
They wanted to ensure that a range of voices from those with lived experience of mental health services was heard in a systematic way by those conducting research into mental health nursing and services. Inspired by the motto ‘Nothing about us, without us’, SUGAR was created. The impact of their work has been significant. The ‘Safewards’ program (http://www.safewards.net/) is just one example of a research SUGAR have been involved in over the years.
Feels daunting
Without this ‘patient involvement’ infrastructure, and the knowledge and experience gained from these resources, the two papers I was involved in would not have been possible. Of course, these papers are only a very small example of what can be achieved with proper patient involvement infrastructure. The real impact is felt across all facets of service provision, as indicated by ELFT being one of only two mental health providers in England to be rated ‘Outstanding’ (highest rating) by the national inspectorate.
Genuine patient power across all aspects of healthcare can feel daunting. It has taken many years to develop the systems described above. However, I believe the benefits of investing in these resources far outweigh the anxiety associated with sharing knowledge and power with the people who use health services.
In Denmark there are clearly some bright spots of patient involvement, for example:
Det brugerinddragende hospital
However, from my brief exposure to the Danish healthcare system, speaking with professionals and patients/carers, my impression is, that patient involvement typically means ‘information sharing’ and ‘consultation’. Is my impression accurate? I’m keen to hear your thoughts…
- What infrastructure is in place in your hospital to support meaningful patient involvement?
- What examples of patient power (partnership, delegated power, patient control) can you share?