At the beginning of 2022 Sundhedsstyrelsen set out their 10-year plan for psychiatry which they described as containing ‘ambitious goals’ to improve psychiatric care in Denmark over the next ten years. Having had the chance to read the document and consider the issues raised and the recommendations presented, I wanted to share some thoughts and reflections.
Firstly, it must be said, that the group developing and writing this plan should be congratulated on the sheer scale of their undertaking; the full version runs at over 200 pages, contains over 350 references and covers a broad range of focus areas and recommendations. A corollary of such breadth and depth is that linked to the nine focus areas are 37 recommendations for change: ambitious indeed.
Within the plan the authors highlight multiple areas of mental health care and treatment which are highly relevant, not just within Denmark, but across the majority of healthcare systems, such as building staffing capacity (recruitment and retention), ensuring coherence and cross-sectoral working, and reducing the stigma associated with mental health diagnoses.
Achieving the recommandations
It is easy to see a red line connecting the nine focus area and the 37 recommendations with these global challenges. Less easy to see in the 10-year plan are any… (dare I say it) “plans” for how these recommendations will be achieved. The authors do state that future documents will include such information, but it strook me that this could be a space – the ‘planning and doing space’ – that I could share some thoughts.
Some of these thoughts were included in the contribution PS! submitted to Sundhedsstyrelsen in November 2021 (Faglige bidrag til 10 års planen for Psykiatri), some were not. The thoughts will be based on observations and experience from both the Danish and the international context, and be framed using improvement science principles, i.e., thinking about the factors we believe are critical to bring about sustained change such as ‘knowing the system’, ‘using data to inform decisions’, understanding the ‘human side of change’, etc.
The international context will be influenced by my experience of working in mental health services in England and undertaking a similar ‘systemic’ change program in a provider organisation – East London NHS Foundation Trust (ELFT). Specifically, shifting from a ‘target’ based, ‘command-and-control’ system of management, to an improvement focused culture.
A journey instigated from terrible circumstances (three patients dying in our care) through to the trust being internationally recognised (and nationally accredited) as outstanding – a summary of which can be read in The Health Foundation – The Improvement Journey. Some of these lessons were applied in the Danish psychiatric improvement program ‘Sikker Psykiatri’ which led to improvements across the four areas of focus: reducing restraint, suicide, and polypharmacy, and improving the physical health of people admitted to inpatient psychiatric services.
Understanding the problem
Typically, when we use improvement science to bring about change, we start by trying to understand the problem from multiple perspectives, by looking at the data, listening to the stories of the stakeholders involved in delivering and using the services we are interested in. However, adopting a ‘whole-system’ perspective can also mean including stakeholders outside the health and social care settings. This could include legal services (police), educational institutions, transport or even the media.
Once collated, this information can be reviewed and then compared to situations elsewhere, i.e., other settings (e.g., cancer treatment) or other countries – a process which I’m pleased to see is specified with the 10-year plan (p79). This process is important in order to form a holistic understanding of both the problem(s) and potential solutions. After all, there’s no point reinventing the wheel.

Discussions with stakeholders (citizens, staff, organisations) to gauge their thoughts on the problems and potential solutions is an important step in the change process. This bottom-up and top-down approach may take time and energy, but the upfront investment tends to pay dividends later down the line (see for example Healthcare Scotland’s approach to developing a national quality strategy).
It also provides an opportunity to share and consider more creative or non-traditional ideas to facilitate changes in mental health services, such as those being tested in Portugal where they have decriminalised drugs to remove it from the criminal justice system and moved it to public health system to support individual and societal harm reduction, or using data from social media to predict mental health needs such as depression, suicide ideation, eating disorders, etc.
The driver diagram
Once there is a shared understanding of the problem, and some potential ideas to support change, we would develop an aim and consider what factors would be critical in achieving that aim. The three questions from the ‘Improvement model’ are helpful: “What are we trying to accomplish?”, “How will we know that a change is an improvement?” and “what change can we make that will result in an improvement?”. When these questions are combined with ‘Plan, Do, Study, Act’ (PDSA) cycles to test changes on a small scale, you have a simple, but powerful tool for accelerating change.
A tool which facilitates understanding the relationship between the aim(s), the nine focus areas and the 37 recommendations is the ‘driver diagram’. The driver diagram is an indispensable tool for mapping out the theory of change. The driver diagram below is based on the content (English translation) from the 10-year plan. On the left of this tool is the overall aim (Question 1. “What are we trying to achieve?”), linked to this are the factors critical to achieving this aim (known as Primary Drivers), which have sub-factors (Secondary Drivers) which are required if the primary drivers are to be achieved. This is a cumulative ‘cause-and-effect’ theory of change, i.e., no single factor will lead to achieving the aim; only in concert will change occur.
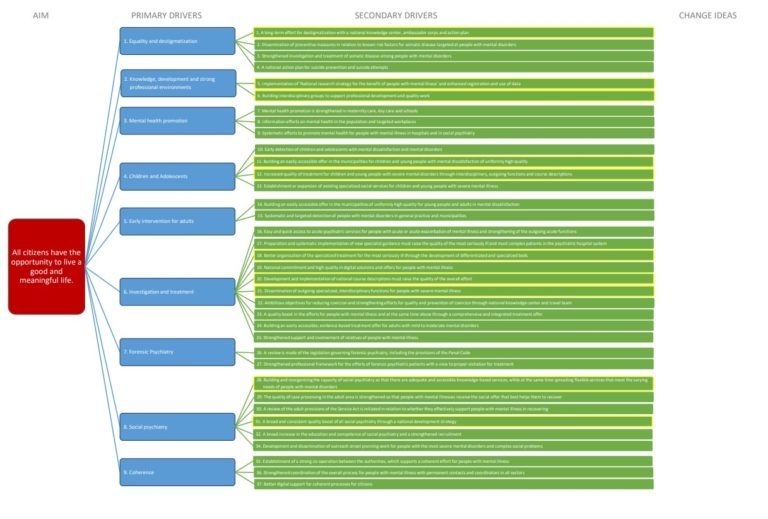
Se driverdiagrammet i stor opløsning
Using data
Often when developing an aim, as in this case, it can appear that the aim is broad or vague, and therefore not ‘SMART’. I don’t see this as hugely problematic. The aim here could be regarded as more ‘campaign-like’ or aspirational. As long as the details of the aim are specified elsewhere, and in the 10-year plan, a detailed breakdown of the aim (Ambitiøse faglige mål) is available and presented in the box 1.
Box 1. Professional goals for the 10-year plan for psychiatry in Denmark
- The mental health of children and young people has improved
- People with mental illness live longer lives with less illness
- People with mental illness are increasingly included and accepted in society
- People with mental illness are retained in jobs, school and education and engage more often in education and employment
- Children, adolescents, and adults with early signs of, or at risk of, developing mental illness receive early, preventive interventions
- Children, adolescents, and adults with mental disorders experience high quality care, involvement, and coherence in their treatment
- Children, young people, and adults with mental illness experience less coercion and use of force
- People with mental illness and concomitant abuse receive a more coherent and effective treatment and are more successful in stopping abuse
- Fewer people with mental illness receive a treatment sentence for crime
- Relatives more often receive the support they need, and their resources are used more actively in their efforts
It is helpful to assign metrics to these goals to clarify exactly what the current situation is (baseline) and what data would indicate successful improvement (Question 2. “How will we know that a change is an improvement?”). This also includes providing clear operational definitions and assigning measures to challenging concepts such as ‘strengthening’ and ‘quality’. Common amongst the recommendations listed. Tracking these data over time (using Statistical Process Control charts) provides a versatile approach which can help diverse stakeholders to manage change in healthcare and improve patients’ health by providing clear indications of change and supporting the overarching administrative organisations with the kind of insight and awareness critical for achieving such ambitious goals.
Testing change ideas
The final elements of the driver diagram are the ‘change ideas’ linked to each of the recommendations. These are connected to Q3 of the improvement model: “what change can we make that will result in an improvement?” In the 10-year plan, the authors have included various examples of change ideas that could be tested, such as implementing IAPT to support achieving ‘Investigation and treatment’ or establishing a new ‘national knowledge centre on de-stigmatisation’ in relation to the focus on ‘Social Psychiatry’.
What will be interesting to see going forward is how these change ideas will be presented, discussed and tested locally. As mentioned previously, simply imposing recommendations ‘from above’ is likely to reduce local ‘buy-in’ and ultimately contribute to less successful change. Which helpfully leads me to my final areas of focus, and one which is often overlooked due to process and system prioritisation, the human side of change.
Local engagement
The evidence from change programs in healthcare is clear, local engagement and ownership is critical. Are frontline staff motivated for change? Do they feel psychologically safe to ask questions, try new ways of working, to collaborate with others outside their teams to support coherence and collaboration? Do they have sufficient knowledge and skills to support the change work?
Related to this, and this an issue we often see with change programs – alongside all the new work and responsibilities, what will be removed? Change often means ‘adding’ (new activities and responsibilities), but health and social care staff are already overburdened with high levels of burnout. So, where in the 10-year plan will there be opportunities for subtraction? All change is ultimately behaviour change. I hope sufficient attention and action is oriented to the humans working and using the services engaged in any change activity.
Using improvement science to support implementation of change
Healthcare is a complex adaptive system; the whole of the system is more than the sum of its parts and characterised by a large number of elements that interact dynamically, sometimes with poor boundary definition and often with histories that influence behaviour. As such methodologies that promote the adoption of changes in health service delivery through iterative planning and practice cycles and subsequent scaling are increasingly of interest internationally.
In this article, I have presented a simplified overview of using improvement science as a method to support the development and implementation of change outlined in the 10-year plan. This approach exploits the learning and engagement gained from testing small scale changes locally, it uses frequently collected data to support understanding and inform decisions. It empowers local change agents and appreciates the importance of the human element involved in change. All factors critical to successful change.
The 10-year plan refers to lessons learnt from previous change plans both within Denmark and abroad, therefore I choose to be optimistic about this plan. However, the words of Shakespeare’s Danish play echo in my mind: “The very substance of the ambitious is merely the shadow of a dream.” Turning the shadows of dreams into the bright light of reality will be the greatest of challenges and where the value will be added.
Fagligt Nyt om patientsikkerhed er et nyhedsbrev, der udgives af PS!, og som udkommer 4-5 gange årligt. Det formidler nyt om de seneste nationale og internationale forskningsresultater, begivenheder, trends og meninger inden for patientsikkerhed.
Tilmeld dig Fagligt Nyt